Resources
- UMMC Research Home
- Research Offices
- Centers and Institutes
- Core Facilities
-
Resources
- Research Resources
- For Researchers
- For Patients
- For Students
- Contact Us
Recent News Stories from UMMC News
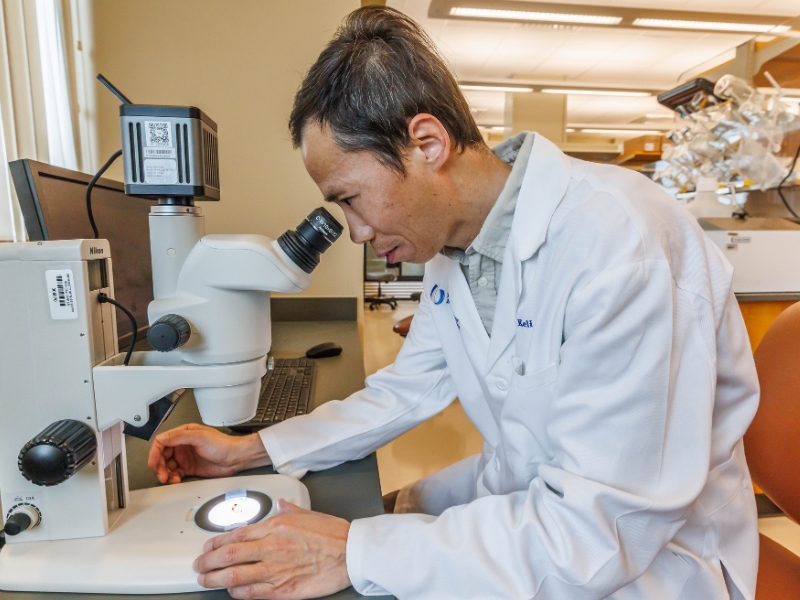
70 Years of Research: Celebrating the Department of Cell and Molecular Biology at UMMC
Monday, January 26, 2026
The UMMC program is working to decode disease at the molecular level, paving the way for breakthroughs in cancer, genomics and precision medicine. Read More

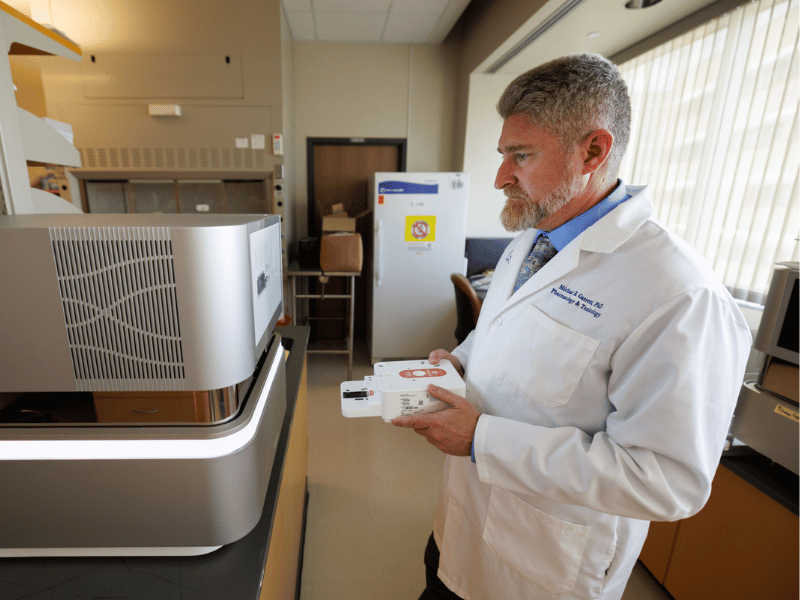
70 Years of Pharmacology: Past, Present, Future
Tuesday, January 20, 2026
As the Department of Pharmacology and Toxicology marks its 70th anniversary, it stands as a powerhouse with a legacy shaped by decades of discovery, leadership and transformation. Read More
CCRI research seeking to unlock mysteries of pancreatic cancer with $1.8M NCI grant
Finding a cell of origin can lead to finding new ways to detect and stop pancreatic ductal adenocarcinoma, which makes up more than 90% of pancreatic cancers.
Published on Monday, December 8, 2025

OAVCR Excellence Awards honor 2025 research accomplishments
Medical Center researchers across disciplines were hailed for their achievements in the past fiscal year, which saw a record number of proposal submissions.
Published on Monday, November 17, 2025

UMMC expands research to address hearing and balance disorders
With a new $11.9 million grant from the NIH, UMMC is creating the Balance and Auditory Research Center. The new center will advance discoveries to improve diagnosis, treatment and rehabilitation in hearing and balance disorders.
Published on Monday, September 22, 2025

Research enterprise surpasses $100M for fiscal 2025
Research studies at UMMC were awarded more than $100 million in fiscal 2025 despite a year marked by funding challenges at the federal level.
Published on Monday, September 8, 2025

UMMC Biobank may reap dividends for improved health statewide
Published on Monday, July 28, 2025
2024-2025 UMMC Promotions and Tenure
Published on Monday, July 7, 2025

Faculty members awarded honor named for medical school legend
Published on Monday, June 30, 2025

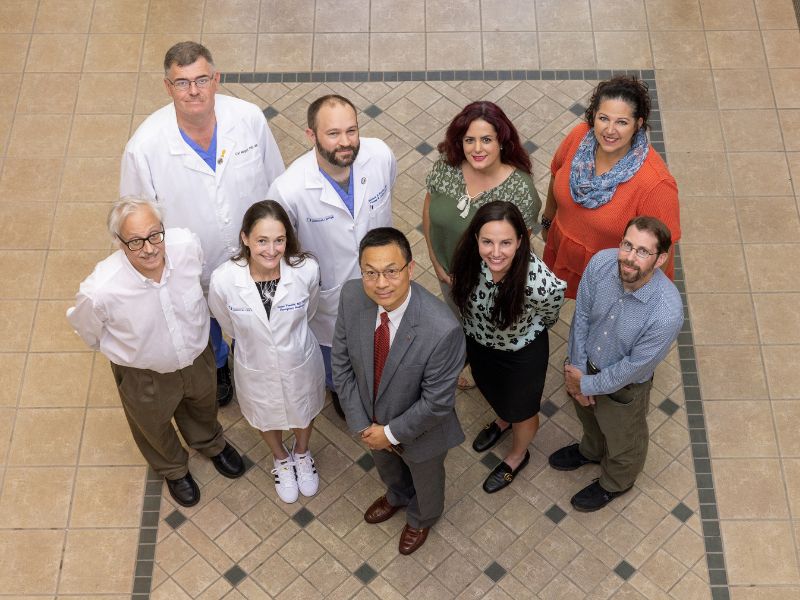
That’s My Job: Research Recruiters
Published on Monday, June 2, 2025
Blue Ridge Institute for Medical Research ranks School of Nursing in top quarter for research funding
Published on Monday, March 10, 2025

Second quarter research grants top $22 million
Published on Monday, February 24, 2025

Annual awards recognize faculty achievements in research
Published on Monday, November 18, 2024

UMMC chosen to lead one of five national hubs for community-led health care research
Published on Monday, October 7, 2024

Dr. John Hall celebrates 50 years of research, teaching at UMMC
Published on Monday, September 16, 2024

Research enterprise reaches nearly $118M for fiscal 2024
Published on Tuesday, September 3, 2024

UMMC launches free tele-mental health clinic for public university students
Published on Monday, August 19, 2024

UMMC receives $1M in federal funds to combat syphilis in Mississippi
Published on Monday, August 5, 2024

UMMC takes heart patient from lethal diagnosis back to athletic powerhouse
Published on Monday, August 5, 2024

UMMC announces new location for ambulatory clinics in Ridgeland
Published on Monday, July 8, 2024

Third quarter grants and awards surpass $42 million
Published on Monday, July 1, 2024

Trauma drug study aims to save lives following severe injuries
Published on Monday, July 1, 2024
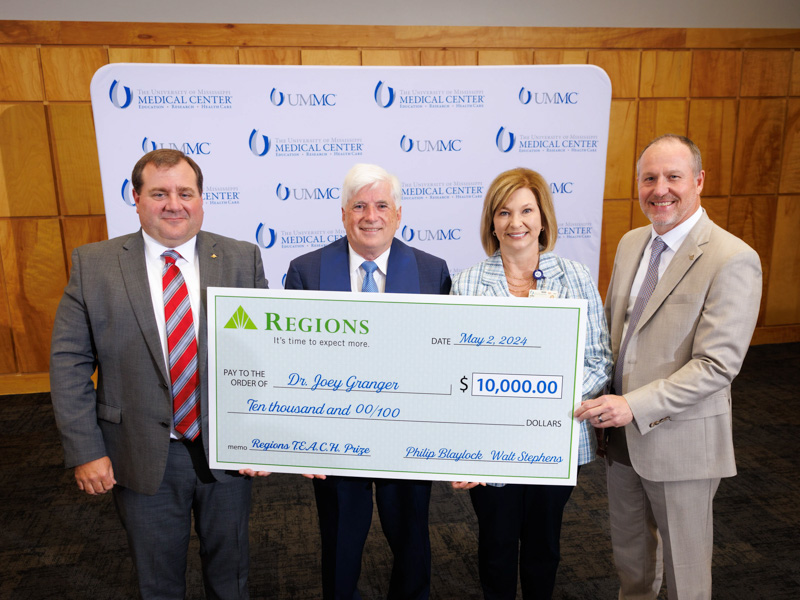
‘Unmatched’ mentor, exemplary educators celebrated
Published on Monday, May 6, 2024
Milestones in UMMC History
Published on Monday, April 22, 2024

#2024UMMCGrad: ER doc masters population health
Published on Monday, April 15, 2024


